As people age, the skin naturally becomes thinner, less elastic, and more fragile. Small injuries that would heal easily in younger skin can become serious wounds in older adults. Understanding the nuances of wound care for elderly with thin skin is critical to prevent tearing, infection, and delayed healing.
This guide covers causes, risks, prevention strategies, dressing selection, step-by-step care, and practical tips tailored to thin elderly skin.
1) Why Elderly Skin Becomes Thin and Fragile
- Decreased collagen and elastin production
- Flattening of the dermal–epidermal junction
- Reduced subcutaneous fat and cushioning
- Thinner capillaries and poorer microcirculation
- Increased dryness and impaired moisture barrier
These changes mean even minor shear, friction, or pressure can lead to tearing, breakdown, or ulceration.
2) Common Wounds in Older Adults with Thin Skin
- Skin tears from minor bumps or friction
- Pressure ulcers / pressure injuries in immobile or bedbound elders
- Abrasions and grazes from falls
- Blisters from friction or ill-fitting shoes
- Superficial lacerations during routine handling

3) Core Principles of Wound Care for Thin Aging Skin
- Gentle handling: Avoid aggressive tapes; favor soft silicone or non-adhesive options.
- Moisture balance: Maintain a moist environment but prevent maceration.
- Protection: Use padding, pressure relief, and friction barriers.
- Infection vigilance: Watch for redness, warmth, odor, or swelling.
- Systemic support: Optimize protein intake, hydration, and comorbidity control.
- Frequent assessment: Inspect daily; adjust dressings as exudate changes.
4) Choosing the Right Dressings
Selecting the right wound dressing for elderly thin skin means finding a balance between protection, gentle adhesion, flexibility, and moisture control. Gentle, atraumatic dressings are key to reducing skin damage during changes and promoting comfort.
Foam Dressings
Ideal for moderate to heavily exudating wounds, foam dressings provide soft cushioning and moisture absorption while minimizing trauma during removal.
Tips: If you want know more about what is foam dressing and how does it work, click here.
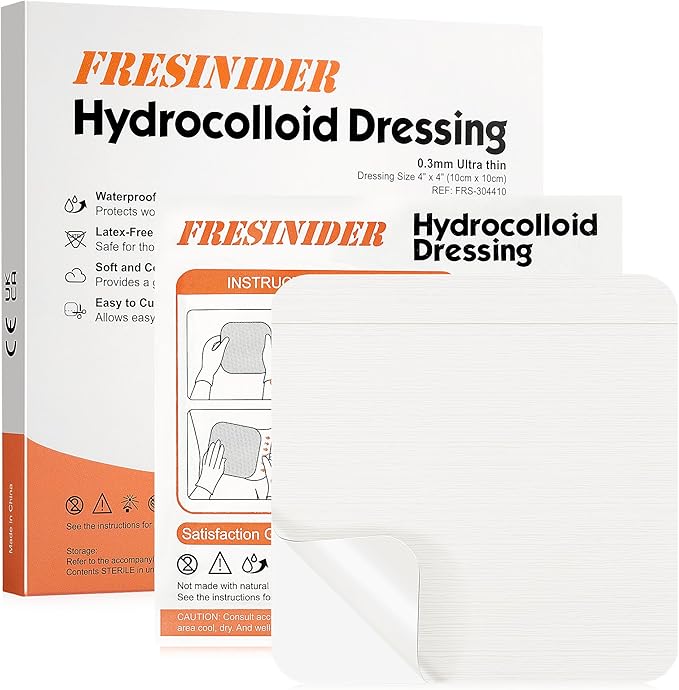
Hydrocolloid Dressings (Thin Formulas)
These dressings create a moist healing environment that supports natural tissue repair and comfort. They work best for shallow wounds or those with light exudate. Because they are occlusive, hydrocolloids should be used carefully on wounds producing moderate to heavy fluid, as excessive moisture may lead to maceration.
Tips: If you want know more about how does hydrocolloid dressings work, click here.
Sacral-Shaped Silicone Foam
For bedridden or chair-bound patients, sacral-shaped foam dressings conform to the curves of the lower back and buttocks, spreading pressure evenly across high-risk areas. They are excellent for preventing pressure injuries in the sacral region, though the edges should be monitored regularly for lifting.
Transparent Film Dressings
Best suited for minor or closed wounds, transparent films are thin, breathable, and easy to remove. They allow caregivers to monitor healing without disturbing the wound bed. However, they have minimal absorption capacity, making them less effective for open or exuding wounds.
Non-Adhesive Pads with Secondary Fixation
For extremely delicate or paper-thin skin, non-adhesive dressings secured with a tubular bandage or soft wrap provide safe protection without direct adhesive contact. This option is preferred when even silicone adhesives might irritate the skin.
5) Step-by-Step Wound Care Protocol
5.1 Clean Gently
- Use sterile saline or a mild wound cleanser.
- Pat dry—never rub.
- Avoid harsh antiseptics (e.g., hydrogen peroxide, iodine) on fragile skin.
5.2 Debridement
Favor autolytic (moisture-assisted) methods. Avoid aggressive mechanical debridement on thin skin.
5.3 Apply the Dressing
- Overlap 1–2 cm onto intact skin.
- Eliminate wrinkles and tension, especially over joints.
- Choose soft silicone or non-adhesive options to minimize trauma at changes.
5.4 Fixation
Use tubular net, soft wraps, or minimal-tack silicone tapes. Secure loosely to prevent constriction.
5.5 Monitor & Change
- Inspect daily for leakage, maceration, edge lifting, or odor.
- Change earlier if saturation or irritation appears.
- Document size, appearance, and exudate level.
5.6 Transition
As healing progresses, step down to lighter, gentler coverings. Once epithelialized, switch to moisturizers and barrier films only.
6) Prevention Tips for Fragile Elderly Skin
- Daily emollients to reduce dryness and brittleness
- Low-friction clothing and bedding
- Reposition immobile patients every 2 hours
- Protect bony prominences with soft padding
- Encourage safe mobility and range-of-motion
- Maintain protein intake, hydration, and micronutrients
7) When to Escalate Care
- Spreading redness, warmth, or malodor
- Rapid rise in pain or exudate
- No improvement within 7–10 days under proper care
- Necrosis or deepening ulceration
- Systemic decline or fever
Seek wound-care specialist input and consider advanced therapies as appropriate.
8) Real-World Considerations
- Adhesive trauma cycle: Even gentle adhesives can cause micro-tears over time—rotate sites and use silicone where possible.
- Polypharmacy & comorbidities: Steroids, anticoagulants, diabetes, and vascular disease may slow healing.
- Ease of use: Choose dressings that caregivers can apply and remove correctly.
- Costs vs outcomes: Advanced dressings may reduce complications and total care costs.
FAQs
Can thin elderly skin heal normally?
Yes—healing may be slower but improves with moisture balance, protection, and gentle dressings.
Are silicone dressings safe?
Soft silicone options are among the gentlest; patch-test if sensitivity is suspected.
How often to change dressings?
Align to exudate level: every 3–5 days for low exudate; more often if moisture increases.
Is film alone enough?
Only for very minor, dry wounds—monitor frequently.