Pressure ulcers—also called bed sores or pressure injuries—are skin and tissue injuries caused by prolonged pressure and shear that limit blood supply and oxygenation. They are common in older adults, immobile patients, and those with chronic illness. Selecting the right dressing is central to prevention and treatment: beyond simply covering a wound, dressings help create an optimal healing environment, protect fragile skin, and support patient comfort.
1. Understanding Pressure Ulcers and the Wound Environment
- Pathophysiology: Pressure + shear → local ischemia → hypoxia → cell death → tissue necrosis.
- Stages: Stage 1 (non-blanchable erythema) to Stage 4 (full-thickness tissue loss), plus unstageable injuries and deep tissue injury (DTI).
- Wound environment: Healing depends on a moist environment, balanced exudate, protection from bacteria, and atraumatic dressing changes.
- Complications: Infection, delayed healing, pain, and reduced quality of life.
2. The Role of Dressings in Pressure Ulcer Care
Effective dressings should:
- Maintain moist wound healing to support tissue repair.
- Absorb and control exudate to prevent maceration of periwound skin.
- Reduce friction and shear at wound edges and pressure points.
- Protect surrounding skin and allow gentle, atraumatic removal.
- Provide a barrier to contaminants and help reduce contamination risk.
- Optionally deliver antimicrobial/therapeutic agents (e.g., silver, honey) when indicated.
- Allow vapor exchange while keeping fluids and bacteria out.
3. Common Types of Pressure Ulcer Dressings
Gauze Dressings
- Pros: Inexpensive, widely available.
- Cons: May adhere to wound bed; poor moisture balance; frequent changes.
- Best for: Temporary coverage or resource-limited settings.

Foam Dressings
- Pros: Highly absorbent; provide cushioning; available with adhesive borders; silicone options minimize trauma.
- Cons: Less suitable for very dry or infected wounds.
- Best for: Moderate-to-heavy exudate; sacral and heel ulcers; pressure-prone areas.

- Provide multilayer protection with a breathable top film
- Soft silicone layer adheres gently, minimizing pain on removal
- Highly absorbent core manages moderate to heavy exudate
- Suitable for surgical wounds, bed sores, diabetic ulcers, and burns
Silicone Foam & Sacral-Shaped Foam
- Pros: Conform to difficult contours (sacrum, buttocks); gentle removal; extended wear time.
- Cons: Opaque design may limit direct wound visualization between changes.
- Best for: Sacral ulcers and preventive use in high-risk patients.
- 5-layer design balances absorption, protection, and breathability
- Soft silicone layer ensures gentle, painless removal
- Sacral shape fits curves of the sacrum and buttocks, preventing pressure injuries
- Suitable for sacral bed sores (Stages 1–4), surgical incisions, and pressure ulcers
Hydrocolloid Dressings
- Pros: Occlusive; maintain moisture; reduce change frequency.
- Cons: Not suitable for heavily exudating or infected wounds.
- Best for: Shallow, low-exuding Stage 2 ulcers.
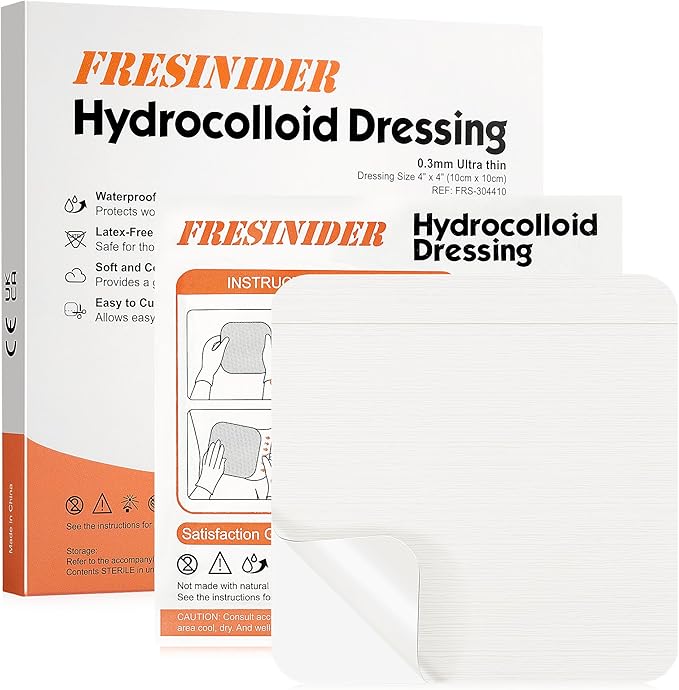
- Forms a soft gel layer with exudate, maintaining a moist healing environment.
- Ultra-thin (0.3mm) and flexible, conforms to curved areas like knees, elbows, and ankles.
- Skin-friendly, latex-free, and breathable for comfortable extended wear.
- Waterproof and cut-to-fit design protects against external contaminants.
- Ideal for shallow wounds, blisters, burns, and acne care.
Hydrogel Dressings
- Pros: Donate moisture; rehydrate necrotic tissue; support autolytic debridement.
- Cons: Low absorption; not for heavy drainage.
- Best for: Dry wounds or wounds with necrotic tissue.
Alginates / Hydrofiber
- Pros: Very absorbent; gel on contact; conform to irregular/cavity wounds.
- Cons: Require a secondary cover; not for dry wounds.
- Best for: Cavity or tunneling ulcers with heavy exudate.
Antimicrobial Dressings (Silver, Honey, Iodine)
- Pros: Help reduce bacterial burden in infected or high-risk wounds.
- Cons: Not for indefinite use; consider potential cytotoxicity; use under clinical guidance.
- Best for: Infected or high-risk ulcers as part of a broader plan.
Advanced / Biological Options
- Examples: Skin substitutes, growth-factor dressings, negative pressure wound therapy (NPWT).
- Pros: Can support stalled or chronic wounds.
- Cons: Higher complexity; specialist care required.
- Best for: Chronic, non-healing ulcers after standard care.
4. How to Choose the Right Dressing
- Wound characteristics: Exudate level, depth, presence of infection, undermining/tunneling, periwound condition.
- Patient factors: Mobility, comorbidities, nutritional status, tolerance and comfort.
- Care setting: Hospital, long-term care, home care; caregiver skill and follow-up capacity.
- Cost & practicality: Realistic change frequency; supply continuity.
- Shape & size: Sacral-shaped dressings for sacrum/buttocks; standard foam for limbs and flat areas.
5. Clinical Evidence & Guidelines
- Guideline themes: NPIAP/EPUAP advocate moist wound healing and individualized selection based on wound assessment.
- Evidence highlights: Foam dressings generally improve comfort and reduce change frequency versus gauze; silver/antimicrobial dressings may help in infected or high-risk wounds but are not for routine use; preventive sacral foam dressings can reduce hospital-acquired pressure injuries in high-risk patients.
- Gaps: Additional randomized trials on cost-effectiveness and sensor/“smart” dressings are needed.
6. Practical Guidance: Using Dressings Effectively
- Prepare the wound: Cleanse with sterile saline; remove necrotic tissue where indicated.
- Apply correctly: Choose appropriate type; ensure an overlap of 1–2 cm onto intact skin.
- Change frequency: Base on exudate and dressing type—daily for gauze; typically 2–7 days for many advanced dressings.
- Monitor: Watch for infection (spreading redness, warmth, odor, increased pain), changes in exudate, and wound dimensions.
- Remove gently: Favor silicone contact layers or moistened removal to minimize trauma.
- Integrate care: Combine with offloading, repositioning, moisture/temperature management, and nutritional support.

7. Cost and Practical Considerations
- Total cost of care: Advanced dressings can reduce nursing time and overall change frequency.
- Supply continuity: Ensure reliable access in hospitals, nursing homes, and home-care settings.
- Comfort & adherence: Atraumatic removal and extended wear improve patient experience and adherence.
Conclusion
There is no single “best” pressure ulcer dressing—selection depends on wound stage, exudate level, infection risk, body location, and care context. Modern options such as silicone foam and sacral-shaped dressings offer strong benefits for protection and comfort, while traditional gauze is best reserved for short-term or resource-limited situations. For optimal outcomes, integrate dressing choice with offloading, routine repositioning, infection control, and sound nutrition.
FAQ
What dressing is best for a Stage 1 pressure ulcer?
Often no dressing is required; protective film or a thin foam can help reduce friction and shear.
How often should dressings be changed?
It depends on exudate and dressing type. Gauze often requires daily changes; many advanced dressings can remain 2–7 days.
Are silver (antimicrobial) dressings recommended?
They may help when infection is present or risk is high, but they are not intended for routine, indefinite use.
Can dressings prevent pressure ulcers?
Yes. In high-risk patients, preventive use of sacral foam dressings—combined with repositioning and offloading—can reduce the incidence of hospital-acquired pressure injuries.





