After surgery, your body begins an intricate healing process that depends heavily on how your incision is protected and managed. Choosing the right post-surgical wound dressing can mean the difference between a smooth recovery and complications like infection or delayed healing.
In this guide, we explain the science of surgical wound healing, how to select the best dressing for your needs, and practical care steps you can follow at home.
What Is a Post-Surgical Wound?
A post-surgical wound (or incision) is a cut made by a surgeon to perform an operation. These wounds are usually closed using sutures, staples, or surgical glue. Even when closed neatly, the surrounding tissue remains fragile for days to weeks.
Surgical incisions vary depending on the procedure: abdominal surgery, orthopedic repair, plastic surgery, or minimally invasive laparoscopic incisions. Each requires a tailored dressing to maintain moisture, absorb exudate, and prevent trauma during movement.
Why the Right Dressing Matters
The correct dressing does more than cover the incision—it protects against bacteria, absorbs excess fluid, and creates a moist healing environment. If the dressing is too dry, it can adhere to the new tissue and tear it during removal. If it’s too moist, the skin around the wound may macerate. That’s why modern wound dressings like silicone foam and hydrocolloid options are increasingly preferred after surgery.
Key Considerations When Choosing a Post-Surgical Dressing
- Exudate level: dry, light, moderate, or heavy drainage.
- Location and mobility: areas like joints need flexible, non-restrictive materials.
- Skin sensitivity: elderly or thin skin may require soft silicone adhesives.
- Duration of use: some dressings can stay in place up to 7 days without disturbance.
- Patient factors: diabetes, smoking, nutrition, and circulation all influence dressing choice.
Types of Dressings for Surgical Wounds
1) Transparent Film Dressings
Thin, flexible films that allow oxygen exchange while keeping bacteria out. Ideal for small, dry incisions or as a protective cover over sutured wounds. Not suitable for heavily draining wounds. Click here to learn more about what is transparent film dressing used for.

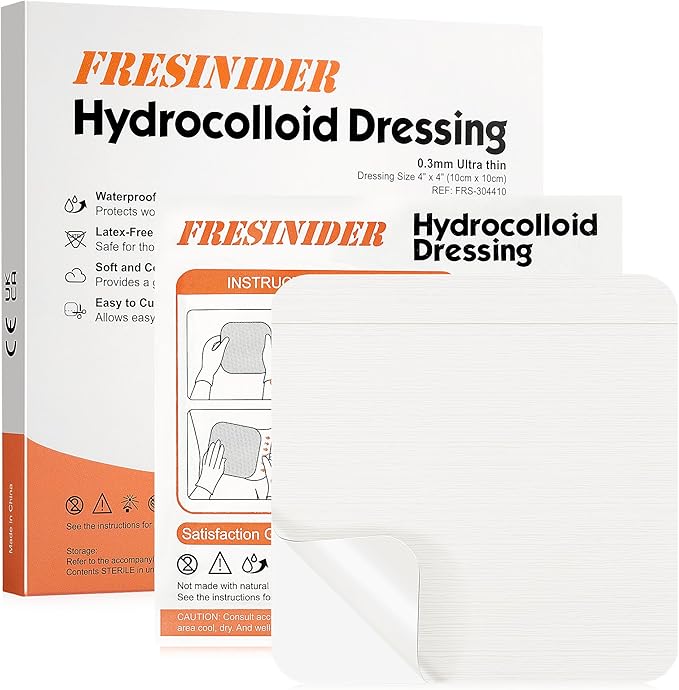
2) Hydrocolloid Dressings
Hydrocolloids form a soft gel when in contact with wound fluid, maintaining a moist environment and protecting against external contamination. Comfortable, waterproof, and allow longer wear time—great for low-exudate surgical sites. Avoid if there’s active infection or heavy drainage, as excess moisture can cause maceration.
Curious about how hydrocolloid dressings promote healing? Explore the science behind them →
3) Silicone Foam Dressings
Foam dressings, especially silicone foam, are excellent for moderate-to-heavy exudate wounds. They absorb drainage while providing cushioning and preventing trauma upon removal. Silicone foam is ideal for surgical sites on joints, the abdomen, or other areas exposed to movement or friction.
New to silicone foam? See how it works and when to use it →
4) Antimicrobial or Silver Dressings
Used for surgical wounds at higher risk of infection (e.g., diabetic, obese, or immunocompromised patients). Silver-infused foams or alginates provide antibacterial protection while maintaining moisture.
5) Negative Pressure Wound Therapy (NPWT)
For complex surgical wounds, NPWT systems (vacuum dressings) may be applied by clinicians to reduce edema and stimulate granulation tissue.
How to Apply and Manage a Surgical Dressing
Step 1 – Clean Gently
- Use sterile saline or the prescribed wound cleanser.
- Avoid alcohol, hydrogen peroxide, or povidone-iodine unless directed.
Step 2 – Inspect the Wound
- Look for redness, swelling, or cloudy drainage before re-dressing.
Step 3 – Apply New Dressing
- Ensure surrounding skin is dry.
- Center the dressing, avoiding folds or air gaps.
Step 4 – Secure Properly
- Use adhesive borders or secondary fixation like tubular gauze.
- Avoid tight taping over sutures.
Step 5 – Monitor Daily
- Replace if saturated or if edges lift.
- Many silicone foam or hydrocolloid dressings can stay in place 3–7 days.

Signs of Complications — When to Call Your Surgeon
- Increasing pain, swelling, or redness
- Yellow or foul-smelling drainage
- Fever or chills
- Separation of wound edges (dehiscence)
- Bleeding that soaks through the dressing
Early attention prevents minor irritation from becoming a major infection.
Evidence-Based Best Practices
Modern advanced dressings—especially silicone foams—can reduce pain during changes, help maintain moisture balance, and lower post-surgical complications compared with traditional gauze. Minimizing dressing disturbance is crucial: “Leave it on unless clinically indicated to change.”
Tips for Patients & Caregivers
- Keep the dressing clean, dry, and intact.
- Wear loose-fitting clothes to avoid friction.
- Do not apply powders, lotions, or ointments unless prescribed.
- For waterproof dressings, you can usually shower—pat dry gently afterward.
- Maintain good nutrition and hydration; protein and vitamins A & C support tissue repair.
FAQs
How long should a surgical dressing stay on?
Typically 2–7 days, depending on drainage and surgeon’s preference.
Can I shower with a post-surgical dressing?
Yes, if it’s waterproof (like silicone foam or hydrocolloid). Pat dry gently afterward.
What type of dressing is best for surgical incisions?
Silicone foam dressings are often recommended—they protect, cushion, and remove gently.
When should I change my dressing early?
If it becomes loose, wet, or soaked through, or if you notice odor or redness.
Conclusion
Proper post-surgical wound dressing isn’t just about covering the incision—it’s about creating the best environment for your body to heal. Choose a dressing that balances protection, absorption, and comfort, and always follow your surgeon’s guidance.